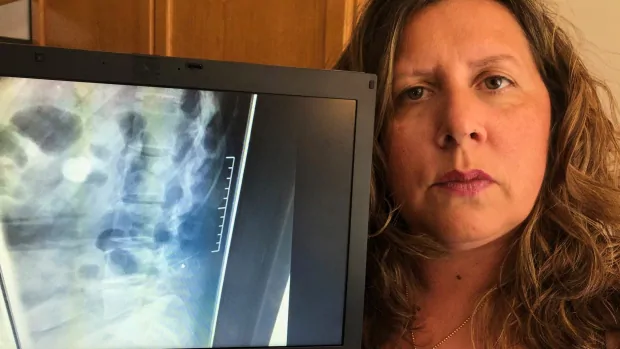
When the pain in her shoulders and weakness in her right leg started two years ago, Giovanna Ippolito thought it was just part of getting older — that’s until the 46-year-old’s doctor ordered an X-ray that showed a five-centimetre long, broken needle embedded in her spine.
It was a medical error that took more than a decade to discover — after medical staff at the time failed to report it.
“When I saw it on the X-ray just protruding out like that … it made me sick to my stomach. It’s scary to know that it’s just sitting there in my spine,” the Bolton, Ont., woman, said of seeing the X-ray in October 2018.
Exactly when the needle was left in Ippolito’s spine is unclear, but she says she’s only had something injected into her back twice — during the birth of her son in 2002 and her daughter in 2004.
Ippolito says she believes the needle broke off when medical staff at Mackenzie Richmond Hill Hospital in nearby Richmond Hill (called York Central Hospital at the time) administered a spinal block or an epidural during one of the births.
She’s now locked in a battle with the hospital for answers and accountability. But experts say, with a system that’s stacked against Canadians harmed by medical errors, it’s likely no one will have to take responsibility.
More than 132,000 patients experienced some kind of medical harm — something both preventable and serious enough to require treatment or a longer hospital stay — in 2018-19, according to the Canadian Institute for Health Information, a Crown corporation that collects information on the country’s health systems.

A five-centimetre needle is found in a woman’s spine at least 16 years after giving birth — which hospital staff failed to report at the time. Experts say with Canada’s medical malpractice system stacked against patients, it’s likely no one will have to take responsibility. 2:22
‘It’s just sheer pain’
Ippolito’s been trying for years to get someone to listen and take action as her symptoms get worse.
“It’s just sheer pain that I get,” she said.
Her doctors can’t directly link the pain she’s experiencing to the needle, and say its location and the scar tissue that’s grown around it make it too dangerous to remove.
In January 2019, she met with hospital officials. But instead of getting answers, she says she was handed a CD-ROM with 174 pages of her patient records, full of medical jargon and illegible, handwritten notes — and told there was no record of the needle breaking, so there was nothing the hospital could do.
It’s possible the needle was left behind without anyone realizing. But patient advocate Francesca Grosso says if medical staff involved in the births noticed half the needle was missing, it’s unacceptable that key piece of information was left out of Ippolito’s records.

It’s unclear who might be responsible. Three anesthesiologists were involved in the births.
That means Ippolito will have a hard time getting anyone to take responsibility under the present system, Grosso says.
“Why was it not identified who actually did what? She’s missing key elements that she doesn’t control,” said Grosso, chair of the advocacy group Patients Canada.
Go Public has learned one of the anesthesiologists involved in Ippolito’s care was cautioned in 2016 by the College of Physicians and Surgeons of Ontario (CPSO) for falling short on care standards, including failing to adequately document his care of patients.
‘Unfair’ battle
Despite Ippolito giving MacKenzie Health permission to answer Go Public’s questions, it declined to do so.
In an email, a spokesperson wrote, “out of respect for this process and confidentiality, we do not comment publicly on any matters related to specific patient cases.”
Generally speaking, the hospital said it meets all “legislated requirements” when looking into cases and that its “processes include case reviews and are accompanied by open discussion with patients, families and/or caregivers as it relates to complaints about medical errors.”

Ippolito says that’s not what happened in her case. Go Public’s investigation found at least one of the anesthesiologists involved wasn’t even asked about the case as part of a review or at any other time.
The other two didn’t respond to our emails, including the anesthesiologist who was cautioned by the college.
After failing to get answers from the hospital, Ippolito contacted the CPSO.
The college tells Go Public that, in order to do an official investigation, it would need the hospital’s help figuring out which of the doctors involved in the births is responsible.
Ippolito also consulted a lawyer and was told there was no point trying to go through the courts.
From 2015-19, only one per cent of patients who initiated malpractice lawsuits won in court; 36 per cent were settled out of court, and more than half — 57 per cent — were dismissed, discontinued or abandoned, according to an annual report by the Canadian Medical Protective Association, the organization that funds doctors’ legal defence. It is funded largely by taxpayer dollars through provinces and territories, which partially reimburse physicians’ CMPA fees.
Most cases don’t even make it to court, according to malpractice lawyer Sloan Mandel.
“It is unfair … these are David-and-Goliath battles. You’re going up against an entity, the Canadian Medical Protective Association, that sets aside billions of dollars to fight cases just like this one,” said Mandel, referring to Ippolito’s situation.
No-fault systems
Those who have looked at the issues say it’s time for a new approach, citing France, New Zealand and other places that use a no-fault compensation system.
Then, patients would be compensated quickly and fairly without having to take doctors to court, according to to Elaine Gibson, a health law professor at Dalhousie University in Halifax.
“A whole system kicks in, an administrative scheme where [patients] receive compensation very quickly,” said Gibson, who wrote a 2016 paper outlining the benefits of a no-fault system.

But provincial and territorial governments don’t seem open to the idea. Go Public asked health ministries across the country if they have considered a no-fault compensation system — most had not.
Ontario says it hired former Justice Stephen Goudge to look into the province’s medical liability system in 2017. The province says he found, “the present fault-based system provides fair and appropriate compensation.”
Quebec doctors came forward in September 2019 supporting a no-fault system, but the province’s Health Ministry says, to date, nothing has come of it.
‘I worry about the future’
Ippolito remembers the day her current doctor showed her the X-ray. She says nurses were coming in and out of her hospital room asking if she was “the woman with the needle in her back.”
She says every time she feels pain, she’s reminded the needle is there and can’t be removed. She worries what that will mean for her future.
“What’s it going to be like in five years?” she said.
“Where’s the accountability? But I won’t go down without a fight.”
Ippolito is now going through the patient ombudsman in Ontario to see if that office can help get the answers she’s looking for — but its scope is limited only to issues Ippolito may have had with the patient relations department at the hospital.

Submit your story ideas
Go Public is an investigative news segment on CBC-TV, radio and the web.
We tell your stories, shed light on wrongdoing, and hold the powers that be accountable.
If you have a story in the public interest, or if you’re an insider with information, contact gopublic@cbc.ca with your name, contact information and a brief summary. All emails are confidential until you decide to Go Public.
Follow @CBCGoPublic on Twitter.

Devoted web advocate. Bacon scholar. Internet lover. Passionate twitteraholic. Unable to type with boxing gloves on. Lifelong beer fanatic.